GALACTIC-HF: Omecamtiv mecarbil in patients with heart failure with reduced ejection fraction
Bottom Line:
In patients with symptomatic HF with reduced ejection fraction (HFrEF), omecamtiv mecarbil did not reduce the risk of death, HF hospitalizations vs placebo over a median of 22 months.
Omecamtiv mecarbil did reduce the primary composite outcome (CV death, HF hospitalization or worsening HF requiring urgent outpatient visit); however, this was driven by urgent outpatient visits & is of unclear clinical importance.
Patients (n=8256):
Included
Chronic HF with NYHA 2-4 & ejection fraction ≤35%
Age 18-85 y
Either
Inpatient: Currently hospitalized for HF
Outpatient: HF hospitalization or ED visit in prior year
Elevated natriuretic peptides
NT-proBNP ≥400 pg/mL if sinus rhythm or ≥1200 pg/mL if afib
BNP ≥125 pg/mL if sinus rhythm or ≥375 pg/mL if afib
Key exclusion
SBP <85 mm Hg or >140 mm Hg
eGFR <20
Untreated severe ventricular arrhythmia, or use of chronic antiarrhythmic therapy (except amiodarone, beta-blockers, digoxin & CCBs)
Certain cardiomyopathies: Severe uncorrected valvular heart disease, hypertrophic or infiltrative cardiomyopathy, active myocarditis, constrictive pericarditis, or clinically significant congenital heart disease
ACS, stroke, TIA or cardiac surgery/intervention within 3 months
Mechanical hemodynamic support or invasive mechanical ventilation in past 7 days
IV inotropes/vasopressors in past 3 days
IV diuretics or vasodilators, supplemental O2, non-invasive mechanical ventilation within 12 hours
Baseline characteristics
Age 64.5 y, 21% female, 78% white
25% enrolled as inpatients, 75% enrolled as outpatients
NYHA 2 (53%), 34 (44%), 4 (3%)
KCCQ-Total Symptom Score: 69/100 (outpatients ~75, inpatients ~53)
LVEF 26.5%
MAGGIC risk score 23 (predicts a 1-year risk of death of ~13%)
T2DM 40%, AF 27%
SBP 116, HR 72, NT-proBNP ~2000, eGFR 59
Meds: ACEI/ARB/ARNI 87% (ARNI 20%), BB 94%, MRA 78%, SGLT2i 2.5%
Devices: CRT 14%, ICD 32%
Intervention: Omecamtiv mecarbil 25-50 mg BID based on therapeutic drug monitoring
Starting dose: 25 mg BID
Dose at 12 weeks: 10% discontinued or missing, 25 mg BID (29%), 37.5 mg BID (14%), 50 mg BID (48%)
Therapeutic drug monitoring protocol from final study protocol
Comparator: Matching placebo
Outcomes at median 22 months
Modest reduction in the risk of a primary outcome (time to first composite of cardiovascular death, HF hospitalization or worsening HF requiring urgent outpatient visit): 37.0% vs 39.1% (HR 0.92, 95% CI 0.86-0.99)
However, no differences in:
Death from any cause: Omecamtiv mecarbil 25.9% vs placebo 25.9%
Hazard ratio (HR) 1.00 (95% confidence interval [CI] 0.92-1.09)
First HF hospitalization: 27.7% vs 28.7% (HR 0.95, 95% CI 0.87-1.03)
Conflicting effect on quality of life with questionable clinical importance:
In outpatients, change vs placebo: -0.5 (95% CI -1.4 to +0.5)
In inpatients, change vs placebo: +2.5 (95% CI +0.5 to +4.5)
No increase in key safety outcomes:
Serious adverse events: 57.7% vs 59.4% (HR 0.97, 0.94-1.01)
Discontinuation due to adverse events: 9.0% vs 9.3% (HR 0.97, 95% CI 0.85-1.11)
Major cardiac ischemic events: 4.9% vs 4.6% (HR 1.06, 95% CI 0.87-1.29)
Ventricular tachyarrhythmia: 7.1% vs 7.4% (HR 0.95, 95% CI 0.82-1.11)
Internal validity: Low risk of allocation, performance, detection & attrition bias
Computer-generated randomization, stratified by setting (inpatient or outpatient)
Allocation concealed by interactive voice/web-response system
Participants, clinicians unaware of treatment assignment & drug plasma concentrations (blinded)
Loss-to-follow-up 2.1% (unknown vital status or died with incomplete follow-up on non-fatal events)
Analysis of the intention-to-treat (ITT) population
Other considerations
Are the results clinically important?
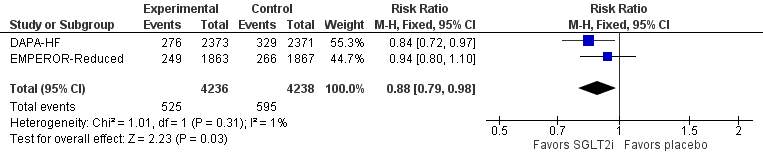
Although administered on top of standard of care, the ~8% relative risk reduction of the primary outcome in this trial is quite modest, especially compared with other interventions for HFrEF
In addition to the uncertain clinical importance of the primary outcome, it is important to note that omecamtiv mecarbil did not reduce the risk of dying, nor did it have a clear effect on HF hospitalizations.
Thus, the main driver of the difference in the primary outcome was worsening HF requiring an urgent outpatient visit, which is far less important than the other 2 components
Generalizability
Overall, the participants of this trial represent a sicker population of HFrEF patients at very high risk of death & hospitalizations, as reflected in the high event rates
Additionally, only a minority of GALACTIC-HF were treated with contemporary HFrEF drugs (ARNI & SGLT2i)
Therefore, the absolute benefits for patients who have less severe HFrEF &/or greater use of ARNIs & SGLT2i are likely to be even smaller
Practical considerations
Cost: Unknown as not yet marketed in Canada/US (as of Dec 29, 2020)
Routine:
Dosing: Requires twice-daily administration.
Monitoring: Requires therapeutic drug monitoring at least once to tailor dose for efficacy & safety - longer term requirements unknown. Does not require any electrolyte/renal monitoring.